Lumbar osteochondrosis is a chronic disease that develops as a result of degenerative-dystrophic processes in the intervertebral disc. The disease spreads and strikes most people between the ages of 25 and 40.
According to statistics, every second adult suffers from back pain at least once in his or her life, while in 95% of cases it is caused by spinal osteochondrosis.
Patients with severe lumbar osteochondrosis, with persistent pain and other manifestations are recognized as temporary disabilities. If within four months their condition does not improve, the issue of setting up a disability group is decided.
Lumbar osteochondrosis is a serious medical and social problem, as the disease mainly affects the oldest person, and in addition, if left untreated, it can lead to the formation of a herniated disc.
Causes and risk factors
Factors that tend to the development of lumbar osteochondrosis are:
- spinal structure anomalies;
- lumbarization - congenital pathology of the spine, characterized by the separation of the first vertebrae from the sacrum and its transformation into the sixth (extra) lumbar;
- sacralization is a congenital pathology in which the fifth lumbar vertebrae merge with the sacrum;
- asymmetric arrangement of intervertebral joint space;
- pathological narrowing of the spinal canal;
- reflects spondiogenic pain (somatic and muscular);
- obesity;
- inactive lifestyle;
- prolonged vibration exposure;
- systematic physical stress;
- smoking.
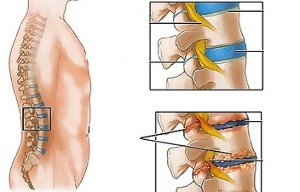
Unpleasant static-dynamic load in combination with one or more risk factors causes a change in the physiological properties of the fibrous nucleus pulposus, which plays a role in absorbing shock and providing mobility of spinal space. This process is based on polysaccharide depolymerization, which causes loss of moisture in the gelatinous core tissue. As a result, the nucleus pulposus, and with it the fibrous disc, loses its elastic properties. Further mechanical stress gives rise to the protrusion of the annulus fibrosus which loses its elasticity. This phenomenon is called protrusion. Cracks appear in the fibrous nucleus, where fragments of the nucleus pulposus fall (prolapse, herniated disc).
Prolonged compression of nerve roots that give breath to certain abdominal organs over time causes a deterioration of their function.
Instability of the spinal segment is accompanied by reactive changes in adjacent vertebral bodies, intervertebral joints, and concomitant spondyloarthrosis. Significant muscle contraction, for example, against the background of physical activity, causes the transfer of the vertebral body and the entrapment of nerve roots with the development of radicular syndrome.
Another cause of pain and neurological symptoms in lumbar osteochondrosis can be osteophytes - bone growths in the processes and body of the vertebrae that cause radicular syndrome or myelopathy compression (compression of the spinal cord).
Forms of disease
Depending on which structure is involved in the pathological process, lumbar osteochondrosis is clinically manifested by the following syndromes:
- reflex- lumbodynia, lumboishalgia, lumbago; develops against a background of excessive pressure on the back muscles;
- compression (spine, vascular, radicular)- compression (compression) of the spinal cord, blood vessels or nerve roots causing its development. An example is lumbosacral radiculitis, radiculoischemia.
Symptoms of lumbar osteochondrosis
In lumbar osteochondrosis, symptoms are determined by which structures are involved in the pathological process.
Lumbago occurs under the influence of hypothermia or excessive physical stress, and sometimes for no apparent reason. The pain appeared suddenly and was of a shooting nature. It gets stronger when sneezing, coughing, turning the body, exercising, sitting, standing, walking. In the supine position, the sensation of pain weakens. Sensitivity and reflexes are maintained, distance of movement in the lumbar spine is reduced.
Note on palpation:
- pain in the lumbar region;
- paravertebral muscle spasm;
- flatten lumbar lordosis, which in many cases is combined with scoliosis.
The nerve root tension syndrome in lumbago is negative. While lifting the legs straight, patients noted an increase in pain in the lumbar region, rather than their appearance in the elongated lower limbs.
Often, with lumbar osteochondrosis, there are recurrent attacks of pain, which each time become stronger and more prolonged.
In lumbodynia, the clinical picture resembles lumbago, but an increase in pain intensity occurs over several days.
With lumboishalgia, the patient complains of pain in the lumbar region that radiates to one or both lower extremities. The pain spread to the back and back of the thighs and never reached the legs.
Lumboishalgia is characterized by vasomotor disorders:
- changes in temperature and skin color of the lower extremities;
- feels hot or cold;
- circulatory disorders.
The development of lumbar compression syndrome is clinically indicated by the following symptoms:
- dermatom hypalgesia;
- shooting pain;
- weakens or completely loses deep reflexes;
- peripheral paresis.
With compression syndrome, the pain is exacerbated by bending the trunk, sneezing and coughing.
Diagnostics
The diagnosis of lumbar osteochondrosis is made based on data from the clinical picture of the disease, laboratory and instrumental research methods.
In a blood test with a background of lumbar osteochondrosis:
- decreased calcium concentration;
- increased ESR;
- increased alkaline phosphatase levels.
In the diagnosis of lumbar osteochondrosis, it is very important for X-ray examination of the spine.
Prolonged compression of nerve roots that give breath to certain abdominal organs over time causes a deterioration of their function.
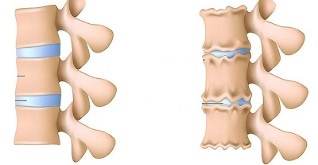
The X-ray mark confirming the diagnosis is:
- changes the configuration of the affected segment;
- pseudospondylolisthesis (displacement of adjacent vertebral bodies);
- cover plate deformation;
- leveling the intervertebral disc;
- uneven intervertebral disc height (spacer symptoms), associated with asymmetric muscle tone.
Also in the diagnosis of lumbar osteochondrosis, if indicated, use:
- myelography, magnetic or magnetic resonance imaging - needed for persistent symptoms, development of neurological deficiencies;
- scintigraphy (study of phosphorus accumulation in the bone system, labeled tech-99) - performed if there is a suspicion of a tumor or infectious process, spinal cord injury.
Differential diagnosis of lumbar osteochondrosis is made with the following diseases:
- spondylolisthesis;
- dishormonal spondylopathy;
- ankylosing spondylitis (ankylosing spondylitis);
- infectious processes (inflammation of the disc, osteomyelitis of the spine);
- neoplastic process (primary tumor of the spine or its metastatic lesions);
- rheumatoid arthritis;
- deformity of osteoarthritis of the hip joint;
- reflected pain (disease of internal organs and large blood vessels).
Treatment of lumbar osteochondrosis
For lumbar osteochondrosis, the following treatment tactics are usually followed:
- bed rest for 2-3 days;
- traction on the affected part of the spine;
- strengthens the back muscles and abdominal muscles (creates a so-called muscle corset);
- effects on pathological myofascial and myotonic processes.
Lumbago occurs under the influence of hypothermia or excessive physical stress, and sometimes for no apparent reason.
In most cases, conservative treatment of lumbar osteochondrosis is performed, including the following:
- muscle infiltration anesthesia with local anesthetic solution;
- taking non-steroidal anti-inflammatory drugs;
- take desensitizing agent;
- vitamin therapy;
- take sedatives and antidepressants;
- manual therapy, massage;
- physiotherapy training;
- acupuncture;
- post-isometric relaxation.
The absolute indications for surgical treatment of lumbar osteochondrosis are:
- acute or subacute spinal cord compression;
- development of cauda equina syndrome, characterized by pelvic organ dysfunction, sensory and movement disorders.
Therapeutic exercises for lumbar osteochondrosis
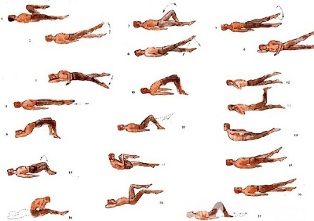
Physical therapy plays an important role in the complex treatment of lumbar osteochondrosis. Regular exercise allows you to normalize the tone of the paravertebral muscles, improve metabolic processes in tissues affected by pathological processes, and, in addition, form a well-developed muscle corset that can support the spine in the correct position, eliminating unnecessary static loadfrom him.
In order for gymnastics for lumbar osteochondrosis to have the greatest impact, the following principles must be followed:
- class order;
- gradual increase in intensity of physical activity;
- avoid overwork during class.
Physiotherapy should be performed under the guidance of experienced instructors, who will select the most effective training for a particular patient and control the truth of its implementation.
According to statistics, every second adult suffers from back pain at least once in his life, while in 95% of cases it is caused by spinal osteochondrosis.
In addition to classes with instructors, you should do daily morning exercises, which include special exercises for lumbar osteochondrosis.
- Relaxation and contraction of the abdominal muscles.Starting position standing, feet shoulder-width apart, arms lowered to the body. Inhale smoothly, relaxing the muscles of the anterior abdominal wall. While exhaling, pull the abdomen as much as possible, tense the abdominal muscles. Exercise should be repeated until mild fatigue appears.
- Movement of the head with bending of the spine.The starting position is on the knees, leaning on the floor with arms outstretched, back straight. Lift your head slowly and bend your back. Hold this position for a few seconds, then return to the starting position smoothly. Repeat at least 10-12 times.
- "Pendulum".Starting position lying on the back, arms along the body, legs bent at right angles to the knee and hip joints. Rotate the legs to the right and left in a swinging pendulum-like motion, trying to reach the floor. In this case, the shoulder blades should not be torn off the floor.
- Bot.The starting position lies on your stomach, arms extended forward. Tear the upper body and legs off the floor, bending at the back. Hold this position for 5-6 seconds and slowly return to the starting position. Running 10 times.
Potential consequences and complications
The main complications of lumbar osteochondrosis are:
- intervertebral hernia formation;
- vegetative-vascular dystonia;
- spondylolysis, spondylolisthesis;
- osteophytosis;
- spondyloarthrosis;
- stenosis of the spinal canal, which causes compression of the spinal cord and can lead to permanent disability and decreased quality of life.
Prolonged compression of nerve roots that give breath to certain abdominal organs over time causes a deterioration of their function. As a result, patients experience intestinal dysfunction (constipation, diarrhea, bloating) and pelvic organs (urinary disorders, erectile dysfunction, frigidity, infertility).
Forecast
Pain syndrome in lumbar osteochondrosis occurs in the form of remission and exacerbation. Lumbago lasts 10-15 days, after which the patient's condition improves, the pain subsides. Good results can be prevented by related secondary diseases. Often, with lumbar osteochondrosis, there are recurrent attacks of pain, which each time become stronger and prolonged.
Physical therapy plays an important role in the complex treatment of lumbar osteochondrosis.
Patients with severe lumbar osteochondrosis, with persistent pain and other manifestations are recognized as temporary disabilities. If within four months their condition does not improve, the issue of setting up a disability group is decided.
Prevention
Prevention of the development of spinal osteochondrosis consists of the following steps:
- quit smoking;
- weight normalization;
- improvement of general physical condition, active lifestyle;
- avoid provocative situations (weight lifting, sudden movements, bends, bends).












































